Knee Arthritis: Overview
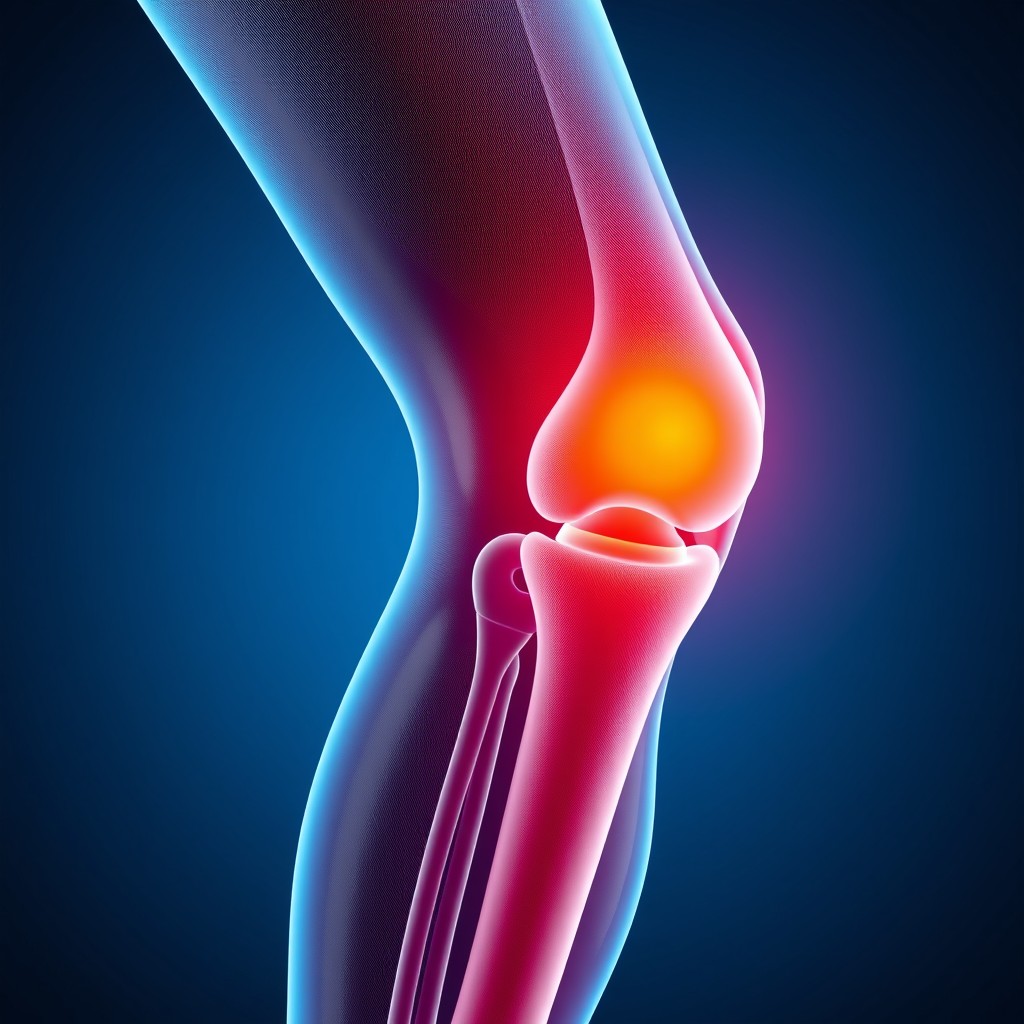
Knee arthritis is a common condition characterized by the inflammation and gradual degeneration of the cartilage in the knee joint. The most prevalent type is osteoarthritis (OA), a "wear and tear" condition where the cartilage that cushions the knee wears away over time, leading to pain, stiffness, and reduced mobility. Other forms include rheumatoid arthritis (RA), an autoimmune condition that causes inflammation of the joint lining, and post-traumatic arthritis, which develops after an injury.
Symptoms of Knee Arthritis:
- Pain in the knee joint (worse after activity or prolonged periods of rest)
- Stiffness, especially in the morning or after sitting
- Swelling and tenderness
- Reduced range of motion
- Clicking or grinding sounds when moving the knee
Treatment of Knee Arthritis
1- Conservative/Non-Surgical Treatments:
Lifestyle Modifications: Weight loss, low-impact exercises (like swimming or cycling) can help reduce stress on the knee.
Medications:
- NSAIDs (Non-steroidal anti-inflammatory drugs) like ibuprofen can reduce inflammation and pain.
- Corticosteroid Injections: Temporary relief of pain and swelling in the joint.
- Hyaluronic Acid Injections: Provides lubrication to ease movement and relieve pain.
Physical Therapy: Strengthening the muscles around the knee to support the joint.
Bracing and Assistive Devices: Knee braces or canes to reduce stress on the joint.
2- Surgical Treatments:
Arthroscopy: Minimally invasive surgery to remove damaged cartilage or bone spurs.
Osteotomy: Bone realignment surgery to shift weight off the damaged portion of the knee.
Partial or Total Knee Replacement (Arthroplasty): Replacement of damaged parts of the knee with prosthetic components.

Cell Therapy for Knee Arthritis
Cell therapy is an emerging treatment for knee arthritis that aims to regenerate damaged tissue, delay the progression of arthritis, and potentially avoid surgery. Cell-based therapies focus on using the body’s own cells or bioengineered cells to heal or regenerate cartilage and other damaged tissues.
1. Stem Cell Therapy:
Stem cells are undifferentiated cells that have the potential to develop into various specialized cells, such as cartilage or bone cells. For knee arthritis, mesenchymal stem cells (MSCs) derived from sources like bone marrow or adipose (fat) tissue are commonly used.
Procedure: Stem cells are harvested from the patient's bone marrow or fat tissue, processed, and then injected into the knee joint.
How it works: Once injected, stem cells can potentially differentiate into cartilage cells and aid in tissue repair, reduce inflammation, and release growth factors that promote healing.
Benefits: Non-invasive, with the potential to repair damaged tissue and improve knee function.
Limitations: The success rates are variable, and while promising, more research is needed to confirm its long-term effectiveness.
2. Platelet-Rich Plasma (PRP) Therapy:
PRP therapy uses a concentrated form of the patient’s own platelets to promote healing.
Procedure: Blood is drawn from the patient, processed to concentrate the platelets, and then injected into the knee joint.
How it works: Platelets release growth factors that help in tissue healing and inflammation reduction.
Benefits: PRP is thought to improve knee pain and function, especially in early arthritis, and is less invasive than surgery.
Limitations: While PRP can reduce symptoms, it may not regenerate cartilage as effectively as stem cell therapy.
3. Chondrocyte Implantation:
This therapy involves using the patient’s own cartilage cells (chondrocytes) to regenerate new cartilage in the knee joint.
Procedure: Cartilage cells are harvested from a non-weight-bearing area of the knee, expanded in a lab, and then re-implanted into the damaged area of the joint.
How it works: Chondrocytes produce cartilage tissue that can repair or replace the damaged cartilage.
Benefits: More targeted at cartilage regeneration and is suitable for younger patients or those with localized cartilage damage.
Limitations: This is a more complex, two-step procedure and may not be suitable for advanced arthritis cases.
Conclusion
Cell therapy for knee arthritis is an exciting and evolving field. While traditional treatments like physical therapy, medications, and surgery address symptoms and manage arthritis progression, cell-based therapies like stem cell and PRP offer the potential for regenerative treatment, focusing on repairing the damaged joint tissue. However, these treatments are still largely considered experimental, and long-term data is still being gathered on their effectiveness.
what we do?
We conducted a project at the Radiology Research Center to examine the effect of injecting mesenchymal stem cells from umbilical cord fat into the knee joint of patients with osteoarthritis using the endovascular method. This study consists of three phases. In phases 1 and 2, the safety of the method and clinical success during the procedure were achieved 100%. No patient experienced any complications during the procedure or after the injection in the follow-up examinations conducted at weeks 0 to 4, and then at months 3, 6, and 12. None of the patients faced issues such as bleeding during the injection. Pulse examinations were regularly performed for all patients over a 24-hour period, and no evidence of tissue ischemia was observed; pulses were full and symmetrical. Arterial and venous color Doppler ultrasound was performed on all patients before discharge, and all patients had complete vascular health in the lower limbs following the injection. No signs of limb ischemia, thrombosis, vascular injury, or any other complications were reported in any of the patients post-injection. The study will continue with phase 3 to assess the effectiveness, following the completion of phases 1 and 2.
If you are interested in collaborating with the Research Center, please fill out and submit the form below.



