Hepatic iron overload and fibrosis in patients with beta thalassemia major after hematopoietic stem cell transplantation: A pilot study
We recommend that regardless of the amount of iron overload in patients with beta thalassemia major that have shown some degree of fibrosis in their liver biopsy before transplantation, appropriate steps should be taken to reduce iron overload as soon as possible after successful transplantation
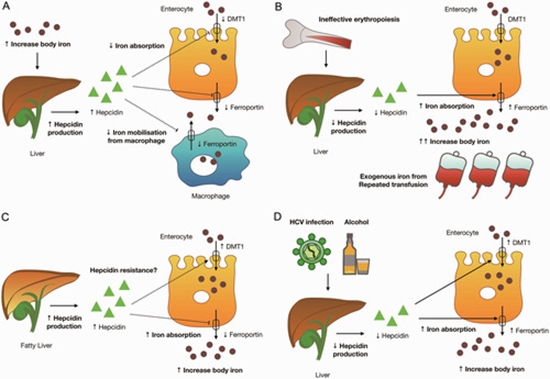
Currently, hematopoietic stem cell transplantation (HSCT) is the only curative option for patients with beta-thalassemia major, but liver iron overload in these patients will not decrease and hepatic fibrosis may still progress despite successful HSCT. Liver biopsy samples were taken from 14 patients (Out of 25 patients) who underwent HSCT. All patients met three criteria: negative HCV antibody, liver fibrosis in samples before HSCT and lack of regular treatment for iron overload after HSCT (Because patients did not consent to phlebotomy or they had not regular follow-up). We evaluated liver fibrosis and liver iron overload by a semi quantitative method, Perls' Prussian blue staining, before and after HSCT. HSCT was successful in all the patients. Liver iron overload did not change after transplant (P=0.61), but hepatic fibrosis progressed after transplant (P=0.01). In patients with beta thalassemia major who previously had some degree of liver fibrosis, HSCT alone cannot reduce liver iron overload and liver fibrosis will increase. We recommend that regardless of the amount of iron overload in patients with beta thalassemia major that have shown some degree of fibrosis in their liver biopsy before transplantation, appropriate steps should be taken to reduce iron overload as soon as possible after successful transplantation.





ارسال به دوستان