Impact of obstetric and surgical factors on isthmocele development: insights from a prospective cohort study

Background: Isthmocele is a defect at the site of the cesarean section scar and is increasingly being recognized as a common complication following cesarean delivery. It may cause abnormal uterine bleeding, pelvic pain, and fertility issues. This study aimed to identify risk factors associated with isthmocele formation after the first cesarean section.
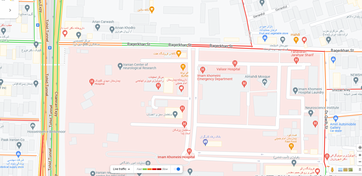
Methods: This prospective cohort study included 262 women aged 14-50 years who underwent their primary cesarean section at Arash Women's Hospital from 2021 to 2024. Previous cesarean deliveries, the history of myomectomy, repeated uterine curettage, and age outside the 14-50 years were exclusion criteria. Demographic, obstetric, surgical, and postoperative data were collected. A transvaginal ultrasound was used for the detection of an isthmocele. Univariate and multivariate logistic regression analyses were performed to identify associated factors with isthmocele formation.
Results: Isthmocele was detected in 19% (n = 50) of patients. Women with isthmocele had higher gestational age at delivery (39.2 ± 0.9 vs. 38.5 ± 1.7 weeks; p = 0.04), shorter delivery intervals (4.6 ± 1.3 vs. 5.2 ± 0.9 years; p = 0.01), more frequent retroverted uterus (28% vs. 11.3%; p = 0.003) and locking suture repair (20% vs. 7.1%; p = 0.005). In multivariable analysis, gestational age (OR = 1.71, 95% CI 1.19, 2.45) and retroverted uterus (OR = 2.82, 95% CI 1.25, 6.35) increased the odds of isthmocele, while longer inter-delivery intervals were protective (OR = 0.65, 95% CI 0.44, 0.97).
Conclusions: Isthmocele is a frequent complication after primary cesarean section. Modifiable factors, such as the timing of delivery, management of infection, inter-pregnancy interval, and surgical technique, should be considered in reducing the risk.




ارسال نظر